- Calls to this hotline are currently being directed to Within Health or Eating Disorder Solutions
- Representatives are standing by 24/7 to help answer your questions
- All calls are confidential and HIPAA compliant
- There is no obligation or cost to call
- Eating Disorder Hope does not receive any commissions or fees dependent upon which provider you select
- Additional treatment providers are located on our directory or samhsa.gov
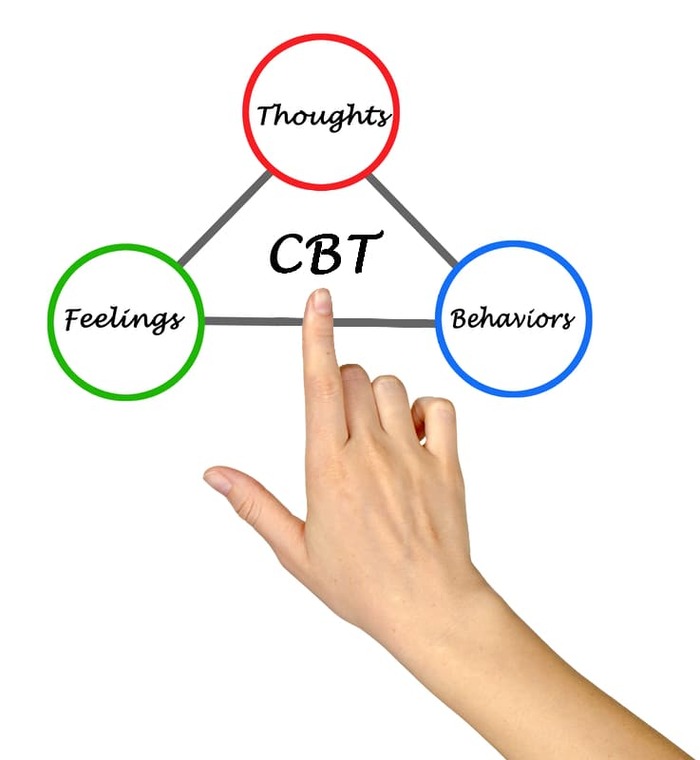
Cognitive Behavioral Therapy (CBT) for Eating Disorders
Eating disorders involve disturbance of eating behavior that leads to “altered consumption or absorption of food that significantly impairs physical health or psychosocial functioning [1].” Cognitive Behavioral Therapy, also known as “CBT,” is the most commonly utilized and evidence-based treatment for most mental health disorders, including eating disorders. How this therapy is used in eating disorder treatment and why it is so effective is important to understand if you are experiencing CBT as a patient or utilizing it as a treatment professional.
What is Cognitive Behavioral Therapy for Eating Disorders?
The foundation of Cognitive Behavioral Therapy is apparent in the name itself and the emphasis of “cognitions,” or, thoughts. CBT ideology comes from the belief that mental and emotional distress is caused by negative, maladaptive, and unhelpful thoughts about oneself, others, and circumstances and the environment around them. CBT posits that one’s thoughts lead to emotions and emotions lead to behaviors. As such, CBT therapy involves altering one’s core beliefs and thoughts in order to then alter emotions and behavior.
In relation to treating disorders, this means supporting those struggling in identifying the beliefs they have about themselves, bodies, appearance, food, exercise, worth, etc. that perpetuate eating disorder behaviors and replacing these with more recovery-focused beliefs. For example, an individual with a core belief that they must be thin in order to be valued would be encouraged to replace these thoughts with ones emphasizing the deeper and more internal aspects of what makes them valuable and worthy.
Main Components of CBT
The American Psychological Association provides a more in-depth look at the foundations of CBT, specifying three foundational principles of the treatment:
- “Psychological problems are based, in part, on faulty or unhelpful ways of thinking.
- Psychological problems are based, in part, on learned patterns of unhelpful behavior.
- People suffering from psychological problems can learn better ways of coping with them, thereby relieving their symptoms and becoming more effective in their lives [2].”
These principles are applied in therapy practice to develop the following skills related to cognitions and behaviors:
- “Learning to recognize one’s distortions in thinking that are creating problems, and then to re-evaluate them in light of reality.
- Gaining a better understanding of the behavior and motivation of others.
- Using problem-solving skills to cope with difficult situations.
- Learning to develop a greater sense of confidence in one’s abilities [2].”
- Gaining an ability to reframe cognitions based on more effective beliefs.
- Recognizing that having a thought does not mean one needs to choose and make decisions based on that thought.
Creating an Eating Disorder Recovery Meal Plan
Creating a meal plan for eating disorder recovery is another important component of treatment outside of the mental work of CBT skills. The most crucial aspect of creating a recovery meal plan is to seek support from a professional. While there may come a time in your recovery that you feel more capable of generating your own meal plan or engaging in Intuitive Eating, in early recovery, having support of a Dietitian or Nutritionist is necessary. These professionals can help you to develop a plan that is best for healing and re-nourishing your body and maintaining appropriate weight restoration and nourishment. Additionally, they can help teach you the skills needed to learn Intuitive Eating principles for future autonomy over eating.
Types of CBT Treatment
CBT principles have been applied to varying therapeutic techniques and manualized approaches in order to take what is so effective about CBT treatment and expand it. Two of the most effective CBT-based treatments are Acceptance and Commitment Therapy (ACT) and Dialectical Behavioral Therapy (DBT) and applying these to eating disorder treatment is showing promising results.
Acceptance and Commitment Therapy (ACT) for Eating Disorders
Acceptance and Commitment Therapy (ACT) is based in CBT with a specific focus on mindfulness skills as well as the concept of “psychological flexibility.” Psychological flexibility involves approaching the current moment as it is and “holding our own thoughts and emotions a bit more lightly, and acting on longer term values and goals rather than short term impulses, thoughts and feelings [3].” In ACT, individuals are encouraged to accept reality as it is and commit themselves to adapting in the way that is most fulfilling to them if they cannot change reality. Individuals in ACT are also encouraged to develop a compassionate relationship with prior negative beliefs which can help them to release these.
Related Reading
Individuals with eating disorders are often rigid in their disordered beliefs, therefore, ACT can help them to find flexibility in their beliefs. It can also support the individual in acknowledging the ineffectiveness of eating disorder beliefs, identifying their highest values, and creating and practicing new beliefs based on these values. Additionally, mindfulness skills can help an individual with an eating disorder connect more fully with their thoughts and body in their recovery journey.
Dialectical Behavior Therapy (DBT) for Eating Disorders
Dialectical Behavior Therapy (DBT) was initially developed to treat Borderline Personality Disorder yet has been found to be incredibly effective with many other mental health diagnoses, including eating disorders. DBT takes the foundations of CBT, however, the focus on the “dialectical,” emphasizes the concepts of acceptance and change. DBT asserts that an individual can be doing their best in any given moment while simultaneously needing to grow and change. This instills in individuals the concept that two things that are seemingly opposing can exist at the same time.
For those with eating disorders, this concept is helpful in combating their rigid and black-and-white thought processes. For example, an individual can acknowledge that their eating disorders once served a purpose for them as a coping skill yet that it is not helpful to them or does not serve them. This concept also helps individuals with eating disorders cope with emotional dysregulation and negative thought-patterns that may tangentially contribute to their eating disorder. Instead of thinking they must choose if they love someone or are mad at them and, therefore, feeling dysregulated and unable to cope, an individual can acknowledge that they love an individual and are angry with them, reducing the stress of having to choose one rigid belief and behave according to that belief.
DBT also teaches valuable skills that are proven helpful in treating eating disorders. These skills are broken-down into 4 categories, all of which are areas that individuals with eating disorders struggle with –
- Mindfulness: Living in and accepting the present moment without judgment or attempting to change it.
- Interpersonal Effectiveness: Communicating thoughts, feelings, and boundaries effectively in a manner that allows the individual to maintain their highest values and the relationship.
- Distress Tolerance: Having an ability to tolerate distressing situations or emotion-states without choosing actions that make the situation worse
- Emotion Regulation: The ability to use necessary skills in-the-moment to regulate emotions appropriately and effectively.
Effectiveness of CBT for Eating Disorders
CBT has proven effective in treating many of the varying eating disorder diagnoses. There are even CBT treatment methods specifically focused on each diagnoses’. One study specifies that CBT-BN (CBT for Bulimia Nervosa) is “the clear leading treatment for bulimia nervosa in adults [4].” This study also explored the effectiveness of varying CBT methodologies in treating anorexia nervosa and found that CBT-E (CBT-Enhanced) “can be used to treat about 60% of outpatients with the disorder and that in these patients about 60% have a good outcome. Interestingly and importantly the relapse rate appears low [4].” Finally, a method of CBT focused specifically on Binge Eating Disorder (BED), simply known as CBT-BED, is found to have a “sustained and marked effect on binge eating [4].”
Due to CBT’s effectiveness and the diverse methodologies the foundations of CBT have become, there are many ways to utilize CBT in eating disorder treatment, even in conjunction with other effective therapies such as exposure-based therapies or family-based treatments.
If you or a loved one are seeking eating disorder support or treatment, a treatment professional or center that utilizes CBT-based practices will likely be most effective.
Additional Eating Disorder Treatment Therapies
- Eating Disorder Therapy
- Acceptance Commitment Therapy (ACT)
- Dialectical Behavioral Therapy (DBT)
- Exposure Response Prevention Therapy (ERP)
- Eye Movement Desensitization Reprocessing (EMDR)
- Interpersonal Psychotherapy (IPT)
- Family-Based Therapy
- Maudsley Method
- Medical Nutrition Therapy (MNT)
- Somatic Experiencing
- Art Therapy
- Body Movement Dance Therapy
- Equine Therapy
- Alternative Methods Stand Up Paddle Board Yoga
Resources
[1] American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). [2] Unknown (2017). What is cognitive behavioral therapy? American Psychological Association. Retrieved from https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral. [3] Collis, R., Archer, R. (2020). What is psychological flexibility? Working with ACT. Retrieved from https://workingwithact.com/what-is-act/what-is-psychological-flexibility/. [4] Murphy, R. et al. (2010). Cognitive behavioral therapy for eating disorders. The Psychiatric Clinic of North America, 33:3.Author: Margot Rittenhouse, MS, LPC, NCC
Page Last Reviewed & Updated on October 29, 2021 by Jacquelyn Ekern, MS, LPC